Hyperparathyroidism
| Hyperparathyroidism | |
|---|---|
 | |
| Thyroid and parathyroid | |
| Specialty | Endocrinology |
| Symptoms | None, kidney stones, weakness, depression, bone pains, confusion, increased urination[1][2][3] |
| Complications | Osteoporosis[2][3] |
| Usual onset | 50 to 60[2] |
| Types | Primary, secondary |
| Causes | Primary: parathyroid adenoma, multiple benign tumors, parathyroid cancer[1][2] Secondary: vitamin D deficiency, chronic kidney disease, low blood calcium[1] |
| Diagnostic method | High blood calcium and high PTH levels[2] |
| Treatment | Monitoring, surgery, intravenous normal saline, cinacalcet[1][2] |
| Frequency | ~2 per 1,000[3] |
Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood.[1][4] This occurs from a disorder either within the parathyroid glands (primary hyperparathyroidism) or as response to external stimuli (secondary hyperparathyroidism).[1] Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium excreted from the bones and flowing into the blood stream in response to increased production of parathyroid hormone.[1] In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones.[1] Other symptoms may include bone pain, weakness, depression, confusion, and increased urination.[1][2] Both primary and secondary may result in osteoporosis (weakening of the bones).[2][3]
In 80% of cases, primary hyperparathyroidism is due to a single benign tumor known as a parathyroid adenoma.[1][2] Most of the remainder are due to several of these adenomas.[1][2] Very rarely it may be due to parathyroid cancer.[2] Secondary hyperparathyroidism typically occurs due to vitamin D deficiency, chronic kidney disease, or other causes of low blood calcium.[1] The diagnosis of primary hyperparathyroidism is made by finding elevated calcium and PTH in the blood.[2]
Primary hyperparathyroidism may only be cured by removing the adenoma or overactive parathyroid glands.[5][1][2] In asymptomatic patients who present with mildly elevated blood calcium levels, with otherwise normal kidneys, and with normal bone density, monitoring may be all that is required.[2] The medication cinacalcet may also be used to decrease PTH levels in those unable to have surgery although it is not a cure.[2] In patients with very high blood calcium levels, treatment may include large amounts of intravenous normal saline.[1] Low vitamin D should be corrected in those with secondary hyperparathyroidism but low Vitamin D pre-surgery is controversial for those with primary hyperparathyroidism.[6] Low vitamin D levels should be corrected post-parathyroidectomy.[2]
Signs and symptoms
[edit]In primary hyperparathyroidism, about 75% of people are "asymptomatic".[1] While most primary patients are asymptomatic at the time of diagnosis, 'asymptomatic' is poorly defined and represents only those without "obvious clinical sequelae" such as kidney stones, bone disease, or hypercalcemic crisis.[5] These "asymptomatic" patients may have other symptoms such as depression, anxiety, gastrointestinal distress, and neuromuscular problems that are not counted as symptoms.[5] The problem is often picked up incidentally during blood work for other reasons, and the test results show a higher amount of calcium in the blood than normal.[3] Many people only have non-specific symptoms.[7]
Common manifestations of hypercalcemia include constipation, vomiting, weakness, lethargy, fatigue, depression, bone pain, muscle soreness (myalgias), joint pain, decreased appetite, feelings of nausea, abdominal pain, pancreatitis, polyuria, polydipsia, cognitive impairment, kidney stones ([nb 1]), vertigo and osteopenia or osteoporosis.[10][11] A history of acquired racquet nails (brachyonychia) may be indicative of bone resorption.[12] Radiographically, hyperparathyroidism has a pathognomic finding of rugger jersey spine.[13] Parathyroid adenomas are very rarely detectable on clinical examination. Surgical removal of a parathyroid tumor eliminates the symptoms in most patients.[citation needed]
In secondary hyperparathyroidism due to lack of vitamin D absorption, the parathyroid gland is behaving normally; clinical problems are due to bone resorption and manifest as bone syndromes such as rickets, osteomalacia, and renal osteodystrophy.[14]
Causes
[edit]Causes of primary hyperparathyroidism include parathyroid adenoma (80% of patients), multiglandular disease usually seen as hyperplasia of the 4 parathyroid glands (15-20% of patients), parathyroid carcinoma (less than 1% of patients).[15] Primary hyperparathyroidism occurs sporadically and most patients do not have a family history.[15] Radiation exposure increases the risk of primary hyperparathyroidism.[1] Additional risk factors include lithium[16] and thiazide diuretics[17] exposure. A number of genetic conditions including multiple endocrine neoplasia syndromes, hyperparathyroidism-jaw tumor syndrome,[18] familial hypocalciuric hypercalcemia,[19] neonatal severe hyperparathyroidism also increase the risk.[1] Parathyroid adenomas have been linked with DDT although a causal link has not yet been established.[20] The most common causes for secondary hyperparathyroidism include vitamin D deficiency, chronic kidney disease, inadequate calcium intake, malabsorption.[21] Tertiary hyperparathyroidism most commonly occurs from prolonged secondary hyperparathyroidism.[22]
Development
[edit]The parathyroid is composed of 4 glands with 2 located superiorly and 2 located inferiorly.[23] The parathyroid glands are located on the posterior thyroid and are derived from the endoderm of the 3rd and 4th pharyngeal pouches.[23] Specifically, the inferior parathyroid glands are derived from the 3rd pharyngeal pouch and the superior parathyroid glands are derived from the 4th pharyngeal pouch dorsal wing.[24] The ultimopharyngeal body is derived from the 4th pharyngeal pouch ventral wing and the parafollicular cells ( C-cells) are derived when the ultimopharyngeal bodies fuse with the posterolateral thyroid.[24] The parathyroid glands separates from the pharyngeal wall and attaches to the posterior thyroid during the 7th week of human embryonic development.[23]
Mechanism
[edit]Normal parathyroid glands measure the ionized calcium (Ca2+) concentration in the blood and secrete parathyroid hormone accordingly; if the ionized calcium rises above normal, the secretion of PTH is decreased, whereas when the Ca2+ level falls, parathyroid hormone secretion is increased.[8]
Regulation of PTH
[edit]Rapid PTH regulation is controlled by the parathyroid G-protein coupled, calcium sensing receptors which responds to fluctuations in serum calcium levels.[25] Alternatively, prolonged changes in serum calcium influences mRNA-binding proteins altering the encoding of PTH mRNA.[26] There are also calcium independent mechanisms which include repression of PTH transcription through 1α,25-dihydroxyvitamin D binding with the vitamin D receptor.[26] Furthermore, 1α,25-dihydroxyvitamin D also has an impact on the expression of calcium-sensing receptors, indirectly affecting PTH secretion.[26]
Effects of PTH on the Bones
PTH stimulates the bones to release calcium through multiple mechanisms. 1) PTH stimulates osteoblasts which increase expression of RANKL which causes differentiation of the osteoblasts into osteocytes.[27] 2) PTH inhibits secretion of osteoprotegerina to allow for osteoclast differentiation.[27] 3) PTH will also directly activate osteoclasts to cause bone resorption through degradation of hydroxyapatite and organic material.[27] This then causes bone to release calcium into the blood.

Effects of PTH on the Kidneys
Calcium reabsorption in the nephron occurs in proximal convoluted tubule and at the ascending Loop of Henle.[28] PTH acts on the distal convoluted tubule and collecting duct to increase calcium reabsorption in the nephron.[28] PTH also acts on the proximal convoluted tubule to decrease phosphate reabsorption to lower the serum phosphate.[28] This decreases formation of insoluble calcium phosphate salts leading to an increase in serum ionized calcium.
Effects of PTH on the Small Intestines
PTH stimulates the production of 1-alpha-hydroxylase in the proximal convoluted tubule.[28] This enzyme activation hydroxylates inactive 25-hydroxycholecalciferol to active vitamin D (1, 25 dihydroxycholecalciferol).[28] Active vitamin D allows for calcium absorption through transcellular and paracellular pathways.[28]
Secondary hyperparathyroidism occurs if the calcium level is abnormally low. The normal glands respond by secreting parathyroid hormone at a persistently high rate. This typically occurs when the 1,25 dihydroxyvitamin D3 levels in the blood are low and hypocalcemia is present. A lack of 1,25 dihydroxyvitamin D3 can result from a deficient dietary intake of vitamin D, or from a lack of exposure of the skin to sunlight, so the body cannot make its own vitamin D from cholesterol.[29] The resulting hypovitaminosis D is usually due to a partial combination of both factors. Vitamin D3 (or cholecalciferol) is converted to 25-hydroxyvitamin D (or calcidiol) by the liver, from where it is transported via the circulation to the kidneys, and it is converted into the active hormone, 1,25 dihydroxyvitamin D3.[8][29] Thus, a third cause of secondary hyperparathyroidism is chronic kidney disease. Here the ability to manufacture 1,25 dihydroxyvitamin D3 is compromised, resulting in hypocalcemia.[citation needed]
Diagnosis
[edit]

The gold standard of diagnosis is the PTH immunoassay. Once an elevated PTH has been confirmed, the goal of diagnosis is to determine the type of hyperparathyroidism (primary, secondary, or tertiary hyperparathyroidism) by obtaining a serum calcium, phosphate, and PTH levels.
| Serum calcium | Phosphate | Vitamin D Level | PTH | Likely type |
|---|---|---|---|---|
| ↑ | ↓ | ↑ | ↑/↔ | Primary hyperparathyroidism[30] |
| ↓/↔ | ↑ | ↓ | ↑ | Secondary hyperparathyroidism[30] |
| ↑ | ↑ | ↓ | ↑ | Tertiary hyperparathyroidism[31] |
Primary hyperparathyroidism has high calcium, vitamin D, and PTH levels and a low phosphate level.[30][31] Secondary hyperparathyroidism has low serum calcium and vitamin D levels, and high phosphate and PTH levels.[30][31] Tertiary hyperparathyroidism has high serum calcium, phosphate, and PTH and low vitamin D levels.[30][31] Tertiary hyperparathyroidism is differentiated from primary hyperparathyroidism by a history of chronic kidney failure and secondary hyperparathyroidism.[citation needed]
Hyperparathyroidism can cause hyperchloremia and increase renal bicarbonate loss, which may result in a normal anion gap metabolic acidosis.[32] ALP level can be elevated due to bone turnover. Additionally further tests can be completed to rule out other causes and complications of hyperparathyroidism including a 24-hour urinary calcium for familial hypocalciuric hypercalcemia, DEXA scan to evaluate for osteoporosis, osteopenia, or fragility fractures, and genetic testing.[33][34][35][36] Additionally a CT scan without contrast or renal ultrasound can be done to assess for nephrolithiasis and/or nephrocalcinosis if there is concern for it.[36]
Differential diagnosis
[edit]Differential diagnoses of hypercalcemia include humoral hypercalcemia of malignancy, renal failure, malignant bone destruction (such as multiple myeloma, metastatic breast cancer, lymphoma), thiazide diuretics, lithium, immobilization, hyperthyroidism, milk alkali syndrome, multiple endocrine adenomatosis syndromes, and granulomatous diseases.[37] Additionally, familial benign hypocalciuric hypercalcamia can present with similar lab changes.[1] In this condition, the calcium creatinine clearance ratio, however, is typically under 0.01 due to the low levels urine calcium.[1]
Blood tests
[edit]Intact PTH
[edit]In primary hyperparathyroidism, parathyroid hormone (PTH) levels are either elevated or "inappropriately normal" in the presence of elevated calcium. Typically, PTH levels vary greatly over time in the affected patient and (as with Ca and Ca++ levels) must be retested several times to see the pattern. The currently accepted test for PTH is intact PTH, which detects only relatively intact and biologically active PTH molecules. Older tests often detected other, inactive fragments. Even intact PTH may be inaccurate in patients with kidney dysfunction.[citation needed] Intact PTH blood tests may be falsely low if biotin has been ingested in the previous few days prior to the blood test.[38]
Calcium levels
[edit]In cases of primary hyperparathyroidism or tertiary hyperparathyroidism, heightened PTH leads to increased serum calcium (hypercalcemia) due to:[citation needed]
- increased bone resorption, allowing the flow of calcium from bone to blood
- reduced kidney clearance of calcium
- increased intestinal calcium absorption
Serum phosphate
[edit]In primary hyperparathyroidism, serum phosphate levels are abnormally low as a result of decreased reabsorption of phosphate in the kidney tubules. However, this is only present in about 50% of cases. This contrasts with secondary hyperparathyroidism and tertiary hyperparathyroidism, in which serum phosphate levels are generally elevated because of kidney disease.[citation needed]
Alkaline phosphatase
[edit]Alkaline phosphatase levels are usually high in hyperparathyroidism due to high bone turn over. In primary hyperparathyroidism, levels may remain within the normal range, but this is inappropriately normal given the increased levels of plasma calcium.[citation needed]
Nuclear medicine
[edit]Nuclear medicine imaging methods are used by surgeons to locate which parathyroid gland is responsible for hyperparathyroidism or to find ectopic parathyroid adenomas, most commonly found in the anterior mediastinum.[citation needed] Historically, technetium sestamibi scintigraphy was the main method used or this indication.[39] Recently 18F-fluorocholine PET/CT tend to be more and more performed due to excellent diagnostic performance.[40][41]
Classification
[edit]Primary
[edit]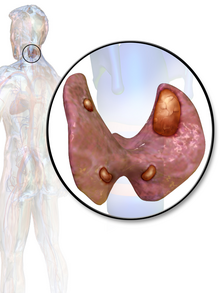
Primary hyperparathyroidism results from a hyperfunction of the parathyroid glands themselves. The oversecretion of PTH is due to a parathyroid adenoma, parathyroid hyperplasia, or rarely, a parathyroid carcinoma. This disease is often characterized by the quartet stones, bones, groans, and psychiatric overtones referring to the presence of kidney stones, hypercalcemia, constipation, and peptic ulcers, as well as depression, respectively.[42][43]
In a minority of cases, this occurs as part of a multiple endocrine neoplasia (MEN) syndrome, either type 1 (caused by a mutation in the gene MEN1) or type 2a (caused by a mutation in the gene RET), which is also associated with the adrenal tumor pheochromocytoma. Other mutations that have been linked to parathyroid neoplasia include mutations in the genes HRPT2 and CASR.[44][45]
Patients with bipolar disorder who are receiving long-term lithium treatment are at increased risk for hyperparathyroidism.[46] Elevated calcium levels are found in 15% to 20% of patients who have been taking lithium long-term. However, only a few of these patients have significantly elevated levels of parathyroid hormone and clinical symptoms of hyperparathyroidism. Lithium-associated hyperparathyroidism is usually caused by a single parathyroid adenoma.[46]
Secondary
[edit]Secondary hyperparathyroidism is due to physiological (i.e. appropriate) secretion of parathyroid hormone (PTH) by the parathyroid glands in response to hypocalcemia (low blood calcium levels). The most common causes are vitamin D deficiency[47] (caused by lack of sunlight, diet or malabsorption) and chronic kidney failure.[citation needed] Vitamin D deficiency can result from malabsorption or decreased vitamin D intake such as with gastric bypass, small bowel disease, pancreatic disease, and dietary causes.[48] Other causes include decreased skin synthesis of vitamin D such as decreased exposure to sunlight and skin disorders. Insufficient vitamin D synthesis such as defective 25-hydroxylation, 1-alpha hydroxylase, and 1-alpha 25-hydroxylation can also contribute to vitamin D deficiency.
Lack of vitamin D leads to reduced calcium absorption by the intestine leading to hypocalcemia and increased parathyroid hormone secretion. This increases bone resorption. In chronic kidney failure the problem is more specifically failure to convert vitamin D to its active form in the kidney. The bone disease in secondary hyperparathyroidism caused by kidney failure is termed renal osteodystrophy.[49]
Tertiary
[edit]Tertiary hyperparathyroidism is seen in those with long-term secondary hyperparathyroidism, which eventually leads to hyperplasia of the parathyroid glands and a loss of response to serum calcium levels. This disorder is most often seen in patients with end-stage kidney disease and is an autonomous activity.[50] Patients with late-stage kidney disease have an increased likelihood of developing tertiary hyperparathyroidism if not promptly corrected.[51] In patients with late-stage kidney disease phosphate levels are elevated which directly affects the parathyroid glands and increases PTH production. Additionally, studies have shown that even in the absence of secondary hyperparathyroidism, those with X-Linked hypophosphatemia rickets who are on phosphate treatment are more susceptible to developing tertiary hyperparathyroidism.[52]
Treatment
[edit]Treatment depends on the type of hyperparathyroidism encountered.
Primary
[edit]Parathyroidectomy is a curative therapy for symptomatic hyperparathyroidism. Additionally, it decrease the risk of nephrolithiasis, osteoporosis, fragility fractures, and improves bone mineral density. Studies have also found that parathyroidectomy for hyperparathyroidism improves fatigue, weakness, depression, and memory. While parathyroidectomy is recommended for all patients with hyperparathyroidism who are symptomatic, indications of surgery for those who are asymptomatic include the following:[53]
- Asymptomatic hyperparathyroidism with any of the following:
- 24-hour urinary calcium >250 mg/day in women and >300 mg/day in men (see footnote, below)
- serum calcium > 1 mg/dl above upper limit of normal
- Creatinine clearance > 30% below normal for patient's age
- Estimated glomerular filtration rate <60 mL/min/1.73 m2
- Bone density > 2.5 standard deviations below peak (i.e., T-score of −2.5)
- People age < 50
- Nephrolithiasis seen on imaging (ultrasound or CT)
A 2020 Cochrane systematic review compared the surgical procedures of minimally invasive parathyroidectomy and classically used bilateral neck exploration, however it did not find one approach to be superior to the other in either benefits or risks.[54]
Surgery can rarely result in hypoparathyroidism.[citation needed]
Secondary
[edit]In patients with secondary hyperparathyroidism, the high PTH levels are an appropriate response to low calcium and treatment must be directed at the underlying cause of this (usually vitamin D deficiency or chronic kidney failure). If this is successful, PTH levels return to normal levels, unless PTH secretion has become autonomous (tertiary hyperparathyroidism).[50] Hyperphosphatemia may be treated by decreasing dietary intake of phosphate. If phosphate remains persistently elevated above 5.5 mg/dL with dietary restriction, then phosphate binders may be used.[55] Vitamin D deficiency may be treated with vitamin D supplementation. However in patients with CKD, patients should not receive vitamin D supplementation if they are elevated serum phosphate levels or have hypercalcemia.[56]
Tertiary
[edit]Parathyroidectomy is indicated in tertiary hyperparathyroidism for patients who have severe osteopenia, severe persistent hypercalcemia (>11.0 mg/ dL), calciphylaxis, bone pain, or pathological fracture.[57] A systematic review found surgical treatment to be superior regarding cure rates than medical therapy with cinacalcet with lower risk of complications.[58]
Calcimimetics
[edit]A calcimimetic (such as cinacalcet) is a potential therapy for some people with severe hypercalcemia and primary hyperparathyroidism who are unable to undergo parathyroidectomy, and for secondary hyperparathyroidism on dialysis.[59][60] Treatment of secondary hyperparathyroidism with a calcimimetic in those on dialysis for CKD does not alter the risk of early death; however, it does decrease the likelihood of needing a parathyroidectomy.[61] Treatment carries the risk of low blood calcium levels and vomiting.[61]
Epidemiology
[edit]In the developed world, between one and four per thousand people are affected.[3] Primary hyperparathyroidism is the most common type.[1] Certain exposures increase the risk of developing primary hyperparathyroidism such as sex and age. It occurs three times more often in women than men and is often diagnosed between the ages of 50 and 60 but is not uncommon before then.[2] The disease was first described in the 1700s.[32] In the late 1800s, it was determined to be related to the parathyroid.[32] Surgery as a treatment was first carried out in 1925.[32] The United States prevalence of primary hyperparathyroidism from 2010 was 233 per 100,000 women and 85 per 100,000 men. Black and white women aged 70–79 have the highest overall prevalence.[62] Secondary hyperparathyroidism is most commonly caused by chronic kidney disease and vitamin D deficiency.[63] The prevalence of vitamin D deficiency is about 50% of the world population and chronic kidney disease prevalence is 15% of the United States population.[51]
History
[edit]The oldest known case was found in a cadaver from an Early Neolithic cemetery in southwest Germany.[64]
Notes
[edit]- ^ Although parathyroid hormone (PTH) promotes the reabsorption of calcium from the kidneys' tubular fluid, thus decreasing the rate of urinary calcium excretion, its effect is only noticeable at any given plasma ionized calcium concentration. The primary determinant of the amount of calcium excreted into the urine per day is the plasma ionized calcium concentration. Thus, in primary hyperparathyroidism, the quantity of calcium excreted in the urine per day is increased despite the high levels of PTH in the blood, because hyperparathyroidism results in hypercalcemia, which increases the urinary calcium concentration (hypercalcuria). Kidney stones are, therefore, often a first indication of hyperparathyroidism, especially since the hypercalcuria is accompanied by an increase in urinary phosphate excretion (a direct result of the high plasma PTH levels). Together, the calcium and phosphate tend to precipitate out as water-insoluble salts, which readily form solid “stones”.[8][9]
References
[edit]- ^ a b c d e f g h i j k l m n o p q r s t Fraser WD (July 2009). "Hyperparathyroidism". Lancet. 374 (9684): 145–58. doi:10.1016/S0140-6736(09)60507-9. PMID 19595349. S2CID 208793932.
- ^ a b c d e f g h i j k l m n o p q "Primary Hyperparathyroidism". NIDDK. August 2012. Archived from the original on 4 October 2016. Retrieved 27 September 2016.
- ^ a b c d e f Michels TC, Kelly KM (August 2013). "Parathyroid disorders". American Family Physician. 88 (4): 249–57. PMID 23944728.
- ^ Allerheiligen DA, Schoeber J, Houston RE, Mohl VK, Wildman KM (April 1998). "Hyperparathyroidism". American Family Physician. 57 (8): 1795–802, 1807–8. PMID 9575320.
- ^ a b c McDow AD, Sippel RS (2018-01-01). "Should Symptoms Be Considered an Indication for Parathyroidectomy in Primary Hyperparathyroidism?". Clinical Medicine Insights. Endocrinology and Diabetes. 11: 1179551418785135. doi:10.1177/1179551418785135. PMC 6043916. PMID 30013413.
- ^ Randle RW, Balentine CJ, Wendt E, Schneider DF, Chen H, Sippel RS (July 2016). "Should vitamin D deficiency be corrected before parathyroidectomy?". The Journal of Surgical Research. 204 (1): 94–100. doi:10.1016/j.jss.2016.04.022. PMID 27451873.
- ^ Taniegra ED (2004-01-15). "Hyperparathyroidism". American Family Physician. 69 (2): 333–339. PMID 14765772.
- ^ a b c Blaine J, Chonchol M, Levi M (July 2015). "Renal control of calcium, phosphate, and magnesium homeostasis". Clinical Journal of the American Society of Nephrology. 10 (7): 1257–72. doi:10.2215/CJN.09750913. PMC 4491294. PMID 25287933.
- ^ Harrison TR, Adams RD, Bennett Jr IL, Resnick WH, Thorn GW, Wintrobe MM (1958). "Metabolic and Endocrine Disorders.". Principles of Internal Medicine (Third ed.). New York: McGraw-Hill Book Company. pp. 575–578.
- ^ Hyperparathyroidism Archived 2011-05-24 at the Wayback Machine. National Endocrine and Metabolic Diseases Information Service. May 2006.
- ^ McKenna K, Rahman K, Parham K (November 2020). "Otoconia degeneration as a consequence of primary hyperparathyroidism". Medical Hypotheses. 144: 109982. doi:10.1016/j.mehy.2020.109982. PMID 32531542. S2CID 219621827.
- ^ Baran R, Turkmani MG, Mubki T (February 2014). "Acquired racquet nails: a useful sign of hyperparathyroidism". Journal of the European Academy of Dermatology and Venereology. 28 (2): 257–9. doi:10.1111/jdv.12187. PMID 23682576.
- ^ "Rugger jersey spine (hyperparathyroidism) | Radiology Reference Article | Radiopaedia.org".
- ^ "Secondary Hyperparathyroidism: What is Secondary Hyperparathyroidism? Secondary Hyperparathyroidism Symptoms, Treatment, Diagnosis - UCLA". www.uclahealth.org. Retrieved 2021-01-18.
- ^ a b Bilezikian JP, Bandeira L, Khan A, Cusano NE (2018-01-13). "Hyperparathyroidism". Lancet. 391 (10116): 168–178. doi:10.1016/S0140-6736(17)31430-7. ISSN 1474-547X. PMID 28923463. S2CID 208790554.
- ^ Szalat A, Mazeh H, Freund HR (February 2009). "Lithium-associated hyperparathyroidism: report of four cases and review of the literature". European Journal of Endocrinology. 160 (2): 317–323. doi:10.1530/EJE-08-0620. ISSN 0804-4643. PMID 19001061.
- ^ Griebeler ML, Kearns AE, Ryu E, Thapa P, Hathcock MA, Melton LJ, Wermers RA (March 2016). "Thiazide-Associated Hypercalcemia: Incidence and Association With Primary Hyperparathyroidism Over Two Decades". The Journal of Clinical Endocrinology & Metabolism. 101 (3): 1166–1173. doi:10.1210/jc.2015-3964. ISSN 0021-972X. PMC 4803175. PMID 26751196.
- ^ du Preez H, Adams A, Richards P, Whitley S (December 2016). "Hyperparathyroidism jaw tumour syndrome: a pictoral review". Insights into Imaging. 7 (6): 793–800. doi:10.1007/s13244-016-0519-0. ISSN 1869-4101. PMC 5110477. PMID 27651062.
- ^ Varghese J, Rich T, Jimenez C (March 2011). "Benign Familial Hypocalciuric Hypercalcemia". Endocrine Practice. 17: 13–17. doi:10.4158/EP10308.RA. PMID 21478088.
- ^ Hu X, Saunders N, Safley S, Smith MR, Liang Y, Tran V, et al. (January 2021). "Environmental chemicals and metabolic disruption in primary and secondary human parathyroid tumors". Surgery. 169 (1): 102–108. doi:10.1016/j.surg.2020.06.010. PMC 7845795. PMID 32771296.
- ^ "Secondary Hyperparathyroidism - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2023-11-02.
- ^ "Tertiary Hyperparathyroidism - an overview | ScienceDirect Topics". www.sciencedirect.com. Retrieved 2023-11-02.
- ^ a b c Rosen RD, Bordoni B (2023), "Embryology, Parathyroid", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32119467, retrieved 2023-11-02
- ^ a b Scharpf J, Kyriazidis N, Kamani D, Randolph G (2016-09-01). "Anatomy and embryology of the parathyroid gland". Operative Techniques in Otolaryngology-Head and Neck Surgery. Surgical Treatment of Hyperparathyroidism. 27 (3): 117–121. doi:10.1016/j.otot.2016.06.003. ISSN 1043-1810.
- ^ Brown EM, MacLeod RJ (2001-01-01). "Extracellular Calcium Sensing and Extracellular Calcium Signaling". Physiological Reviews. 81 (1): 239–297. doi:10.1152/physrev.2001.81.1.239. ISSN 0031-9333. PMID 11152759.
- ^ a b c Kumar R, Thompson JR (February 2011). "The Regulation of Parathyroid Hormone Secretion and Synthesis". Journal of the American Society of Nephrology. 22 (2): 216–224. doi:10.1681/ASN.2010020186. ISSN 1046-6673. PMC 5546216. PMID 21164021.
- ^ a b c Silva BC, Bilezikian JP (June 2015). "Parathyroid hormone: anabolic and catabolic actions on the skeleton". Current Opinion in Pharmacology. 22: 41–50. doi:10.1016/j.coph.2015.03.005. PMC 5407089. PMID 25854704.
- ^ a b c d e f Arnaud CD, Tenenhouse AM, Rasmussen H (March 1967). "Parathyroid Hormone". Annual Review of Physiology. 29 (1): 349–372. doi:10.1146/annurev.ph.29.030167.002025. ISSN 0066-4278. PMID 5335437.
- ^ a b Stryer L (1995). Biochemistry (Fourth ed.). New York: W.H. Freeman and Company. p. 707. ISBN 0-7167-2009-4.
- ^ a b c d e Le T, Bhushan V, Sochat M, Kallianos K, Chavda Y, Zureick AH, Kalani M (2017). First aid for the USMLE step 1 2017. New York: Mcgraw-Hill Education. ISBN 978-1-259-83763-0.
- ^ a b c d "Primary Hyperparathyroidism: A Case-based Review | Clinician Reviews". www.mdedge.com. Retrieved 2023-11-09.
- ^ a b c d Gasparri G, Camandona M, Palestini N (2015). Primary, Secondary and Tertiary Hyperparathyroidism: Diagnostic and Therapeutic Updates. Springer. ISBN 978-88-470-5758-6. Archived from the original on 2017-09-08.
- ^ Minisola S, Arnold A, Belaya Z, Brandi ML, Clarke BL, Hannan FM, Hofbauer LC, Insogna KL, Lacroix A, Liberman U, Palermo A, Pepe J, Rizzoli R, Wermers R, Thakker RV (November 2022). "Epidemiology, Pathophysiology, and Genetics of Primary Hyperparathyroidism". Journal of Bone and Mineral Research. 37 (11): 2315–2329. doi:10.1002/jbmr.4665. ISSN 0884-0431. PMC 10092691. PMID 36245271. S2CID 251340431.
- ^ Lee JY, Shoback DM (October 2018). "Familial hypocalciuric hypercalcemia and related disorders". Best Practice & Research Clinical Endocrinology & Metabolism. 32 (5): 609–619. doi:10.1016/j.beem.2018.05.004. PMC 6767927. PMID 30449544.
- ^ Eastell R, Brandi ML, Costa AG, D'Amour P, Shoback DM, Thakker RV (October 2014). "Diagnosis of Asymptomatic Primary Hyperparathyroidism: Proceedings of the Fourth International Workshop". The Journal of Clinical Endocrinology & Metabolism. 99 (10): 3570–3579. doi:10.1210/jc.2014-1414. ISSN 0021-972X. PMID 25162666.
- ^ a b "A condition that causes an imbalance of calcium in the body-Hyperparathyroidism - Diagnosis & treatment". Mayo Clinic. Retrieved 2023-11-09.
- ^ Allerheiligen DA, Schoeber J, Houston RE, Mohl VK, Wildman KM (1998-04-15). "Hyperparathyroidism". American Family Physician. 57 (8): 1795–1802. PMID 9575320.
- ^ Waghray A, Milas M, Nyalakonda K, Siperstein AE (2013). "Falsely low parathyroid hormone secondary to biotin interference: a case series". Endocrine Practice. 19 (3): 451–5. doi:10.4158/EP12158.OR. PMID 23337137.
- ^ Neish AS, Nagel JS, Holman BL. "Parathyroid Adenoma". BrighamRAD Teaching Case Database. Archived from the original on 2011-07-16.
- ^ Giovanella L, Bacigalupo L, Treglia G, Piccardo A (February 2021). "Will 18F-fluorocholine PET/CT replace other methods of preoperative parathyroid imaging?". Endocrine. 71 (2): 285–297. doi:10.1007/s12020-020-02487-y. ISSN 1355-008X. PMID 32892309.
- ^ Schweighofer-Zwink G, Hehenwarter L, Rendl G, Rettenbacher L, Langsteger W, Beheshti M, Pirich C (February 2019). "Darstellung und Lokalisation von Nebenschilddrüsenadenomen mit F‑18 Cholin PET/CT". Wiener Medizinische Wochenschrift (in German). 169 (1–2): 15–24. doi:10.1007/s10354-018-0660-0. ISSN 0043-5341. PMID 30264384.
- ^ Carroll MF, Schade DS (May 2003). "A practical approach to hypercalcemia". American Family Physician. 67 (9): 1959–66. PMID 12751658. Archived from the original on 21 August 2014.
his constellation of symptoms has led to the mnemonic "Stones, bones, abdominal moans, and psychic groans," which is used to recall the signs and symptoms of hypercalcemia, particularly as a result of primary hyperparathyroidism.
- ^ McConnell TH (2007). The Nature of Disease: Pathology for the Health Professions. Lippincott Williams & Wilkins. p. 466. ISBN 978-0-7817-5317-3.
"Stones" refers to kidney stones, "bones" to associated destructive bone changes, "groans" to the pain of stomach and peptic ulcers that occur in some cases, and "moans" to the depression that frequently accompanies the disease and is often its first and most prominent manifestation.
- ^ Marx SJ (2011). "Hyperparathyroid genes: sequences reveal answers and questions". Endocrine Practice. 17 (Suppl 3): 18–27. doi:10.4158/EP11067.RA. PMC 3484688. PMID 21454225.
- ^ Sulaiman L, Nilsson IL, Juhlin CC, Haglund F, Höög A, Larsson C, Hashemi J (June 2012). "Genetic characterization of large parathyroid adenomas". Endocrine-Related Cancer. 19 (3): 389–407. doi:10.1530/ERC-11-0140. PMC 3359501. PMID 22454399.
- ^ a b Pomerantz JM (2010). "Hyperparathyroidism Resulting From Lithium Treatment Remains Underrecognized". Drug Benefit Trends. 22: 62–63. Archived from the original on 2010-07-01.
- ^ Lips P (August 2001). "Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications". Endocrine Reviews. 22 (4): 477–501. doi:10.1210/edrv.22.4.0437. PMID 11493580.
- ^ Compher CW, Badellino KO, Boullata JI (February 2008). "Vitamin D and the Bariatric Surgical Patient: A Review". Obesity Surgery. 18 (2): 220–224. doi:10.1007/s11695-007-9289-6. ISSN 0960-8923. PMID 18176832. S2CID 24573934.
- ^ Eckardt KU, Kasiske BL (August 2009). "KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)". Kidney International Supplements. 76 (113). Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group: S1–130. doi:10.1038/ki.2009.188. PMID 19644521.
- ^ a b "Hyperparathyroidism". The Lecturio Medical Concept Library. Retrieved 25 July 2021.
- ^ a b van der Plas WY, Noltes ME, van Ginhoven TM, Kruijff S (December 2020). "Secondary and Tertiary Hyperparathyroidism: A Narrative Review". Scandinavian Journal of Surgery. 109 (4): 271–278. doi:10.1177/1457496919866015. ISSN 1457-4969. PMID 31364494. S2CID 198999770.
- ^ Mäkitie O, Kooh SW, Sochett E (February 2003). "Prolonged high-dose phosphate treatment: a risk factor for tertiary hyperparathyroidism in X-linked hypophosphatemic rickets". Clinical Endocrinology. 58 (2): 163–168. doi:10.1046/j.1365-2265.2003.01685.x. ISSN 0300-0664. PMID 12580931. S2CID 20053408.
- ^ Bilezikian JP, Silverberg SJ (April 2004). "Clinical practice. Asymptomatic primary hyperparathyroidism". The New England Journal of Medicine. 350 (17): 1746–51. doi:10.1056/NEJMcp032200. PMC 3987990. PMID 15103001.
- ^ Ahmadieh H, Kreidieh O, Akl EA, El-Hajj Fuleihan G (2020-10-21). Cochrane Metabolic and Endocrine Disorders Group (ed.). "Minimally invasive parathyroidectomy guided by intraoperative parathyroid hormone monitoring (IOPTH) and preoperative imaging versus bilateral neck exploration for primary hyperparathyroidism in adults". Cochrane Database of Systematic Reviews. 10 (10): CD010787. doi:10.1002/14651858.CD010787.pub2. PMC 8094219. PMID 33085088.
- ^ Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, McCann L, Moe SM, Shroff R, Tonelli MA, Toussaint ND, Vervloet MG, Leonard MB (July 2017). "Executive summary of the 2017 KDIGO Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) Guideline Update: what's changed and why it matters". Kidney International. 92 (1): 26–36. doi:10.1016/j.kint.2017.04.006. hdl:1805/15063. PMID 28646995.
- ^ Andrassy KM (September 2013). "Comments on 'KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease'". Kidney International. 84 (3): 622–623. doi:10.1038/ki.2013.243. ISSN 0085-2538. PMID 23989362.
- ^ Palumbo V, Damiano G, Messina M (2021-04-30). "Tertiary hyperparathyroidism: a review". La Clinica Terapeutica. 172 (3): 241–246. doi:10.7417/CT.2021.2322. ISSN 1972-6007. PMID 33956045.
- ^ Dulfer RR, Franssen GJ, Hesselink DA, Hoorn EJ, van Eijck CH, van Ginhoven TM (2017-05-18). "Systematic review of surgical and medical treatment for tertiary hyperparathyroidism". British Journal of Surgery. 104 (7): 804–813. doi:10.1002/bjs.10554. ISSN 0007-1323. PMID 28518414. S2CID 35176289.
- ^ "Sensipar: Highlights of Prescribing Information" (PDF). Amgen Inc. Archived (PDF) from the original on 2014-10-05. Retrieved 2014-10-29.
- ^ Ott SM (April 1998). "Calcimimetics--new drugs with the potential to control hyperparathyroidism". The Journal of Clinical Endocrinology and Metabolism. 83 (4): 1080–2. doi:10.1210/jcem.83.4.4799. PMID 9543121. S2CID 22067453.
- ^ a b Ballinger AE, Palmer SC, Nistor I, Craig JC, Strippoli GF (9 December 2014). "Calcimimetics for secondary hyperparathyroidism in chronic kidney disease patients". The Cochrane Database of Systematic Reviews. 2014 (12): CD006254. doi:10.1002/14651858.CD006254.pub2. PMC 10614033. PMID 25490118.
- ^ Yeh MW, Ituarte PH, Zhou HC, Nishimoto S, Amy Liu IL, Harari A, Haigh PI, Adams AL (2013-03-01). "Incidence and Prevalence of Primary Hyperparathyroidism in a Racially Mixed Population". The Journal of Clinical Endocrinology & Metabolism. 98 (3): 1122–1129. doi:10.1210/jc.2012-4022. ISSN 0021-972X. PMC 3590475. PMID 23418315.
- ^ Saliba W, El-Haddad B (2009-09-01). "Secondary Hyperparathyroidism: Pathophysiology and Treatment". The Journal of the American Board of Family Medicine. 22 (5): 574–581. doi:10.3122/jabfm.2009.05.090026. ISSN 1557-2625. PMID 19734404. S2CID 1411281.
- ^ Zink AR, Panzer S, Fesq-Martin M, Burger-Heinrich E, Wahl J, Nerlich AG (January 2005). "Evidence for a 7000-year-old case of primary hyperparathyroidism". JAMA. 293 (1): 40–2. doi:10.1001/jama.293.1.40-c. PMID 15632333.
External links
[edit]- Overview Archived 2011-05-24 at the Wayback Machine at Endocrine and Metabolic Diseases Information Service
- Insogna KL (September 2018). "Primary Hyperparathyroidism". The New England Journal of Medicine (Review). 379 (11): 1050–1059. CiteSeerX 10.1.1.322.5883. doi:10.1056/NEJMcp1714213. PMID 30207907. S2CID 205069527.
